Jarvis Americas Measles Outbreak Avoidable
Jarvis Americas measles outbreak was entirely avoidable. This wasn’t a natural disaster; it was a preventable crisis fueled by factors like low vaccination rates, misinformation, and a breakdown in public trust. This exploration delves into the causes, preventive measures, impact, and public health messaging surrounding this tragedy, examining how a preventable health crisis can unravel communities and highlight the crucial role of effective communication and international cooperation in public health.
The outbreak highlighted the devastating consequences of declining vaccination rates and the insidious spread of misinformation. Understanding the contributing factors and developing strategies to prevent future outbreaks are crucial. This article analyzes the contributing factors, preventive measures, impact, and effective public health messaging strategies.
Measles Outbreak Causes
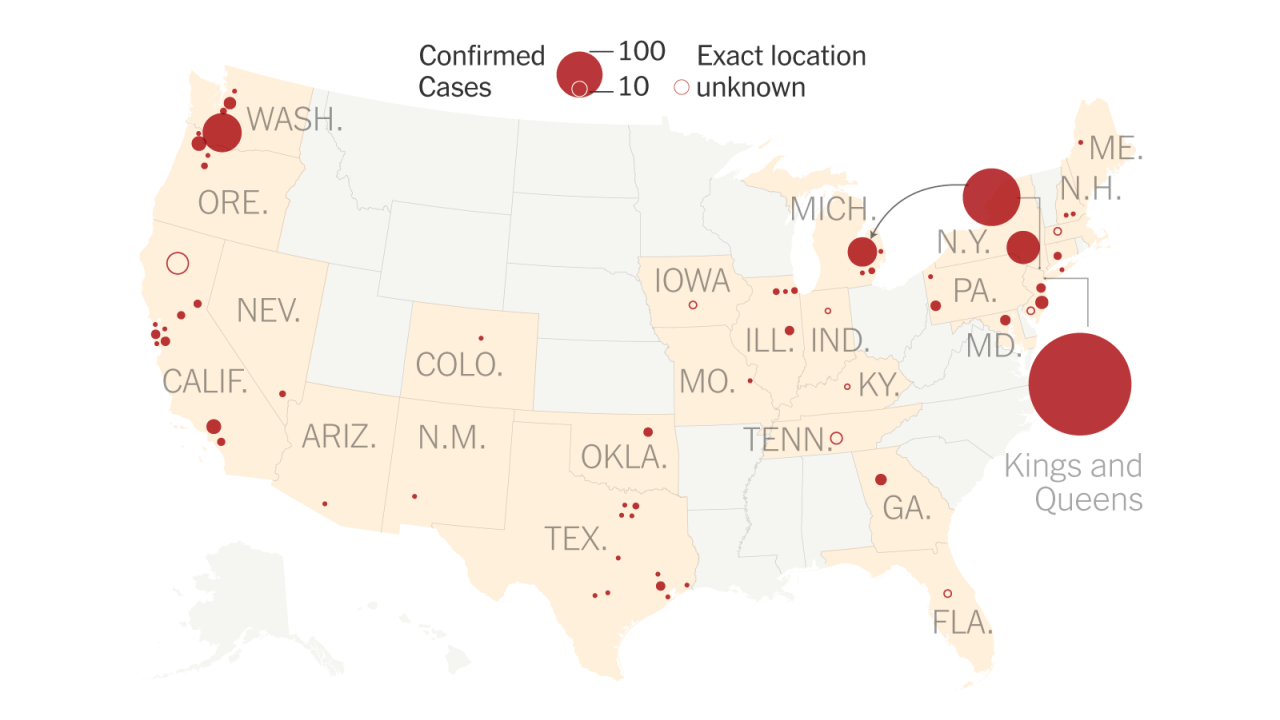
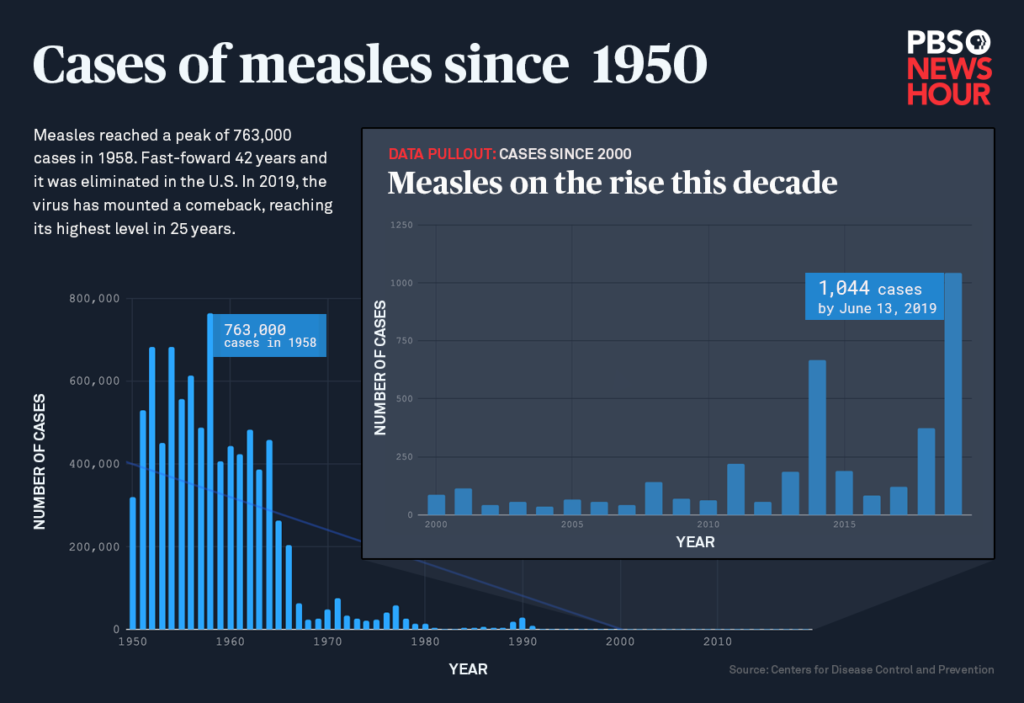
The recent measles outbreak in the Americas serves as a stark reminder of the importance of vaccination and public health measures. While the outbreak has been largely contained, understanding the factors that contributed to its spread is crucial for preventing future outbreaks. The interconnectedness of various factors, from declining vaccination rates to the spread of misinformation, highlights the complexity of public health challenges.The resurgence of measles underscores the critical role of maintaining high vaccination coverage and robust public health infrastructure.
Failure to address these factors can lead to devastating consequences for vulnerable populations.
Contributing Factors to the Outbreak
Several intertwined factors fueled the measles outbreak in the Americas. Low vaccination rates, the spread of misinformation, and socio-political factors all played significant roles. The lack of herd immunity, particularly in communities with lower vaccination coverage, created an environment ripe for the virus to spread rapidly.
Role of Vaccination Rates and Community Immunity
Vaccination rates are a key indicator of a population’s vulnerability to outbreaks. Measles is a highly contagious disease, and outbreaks are more likely to occur when a substantial portion of the population is not vaccinated. This reduced “herd immunity” weakens the protective shield against the disease, allowing it to spread more easily. The recent outbreaks demonstrate how quickly measles can spread through susceptible populations.
Impact of Misinformation and Distrust in Public Health Measures
The spread of misinformation and distrust in public health measures significantly contributed to the outbreak. Misinformation campaigns, often disseminated online, cast doubt on the safety and efficacy of vaccines, leading some parents to choose not to vaccinate their children. This mistrust created pockets of unvaccinated individuals, creating a perfect breeding ground for outbreaks. Cases like the anti-vaccine movement in the United States serve as stark examples.
Socio-political Factors Influencing the Outbreak
Socio-political factors can influence vaccination rates and public health outcomes. Factors like socioeconomic disparities, access to healthcare, and political polarization can all contribute to health disparities, which in turn affect vaccination rates. Cultural beliefs and community norms can also play a role in decisions around vaccination.
The Jarvis America measles outbreak was a total tragedy, and frankly, entirely avoidable. Proper public health measures are crucial, but sometimes, even with the best intentions, things can go wrong. Fortunately, learning from these mistakes is key. Understanding how to build a basic streaming setup, like the ones used by many news outlets to disseminate information, can be incredibly helpful in a crisis like this.
This build basic streaming setup might not directly prevent future outbreaks, but a better understanding of communication channels could improve public awareness and response times in future emergencies. Ultimately, preventing outbreaks like the Jarvis America measles outbreak hinges on proactive measures and a strong understanding of public health protocols.
Specific Measures Taken by Health Authorities
In response to the outbreak, health authorities implemented various measures. These included intensified vaccination campaigns, increased surveillance and contact tracing, and public health education initiatives aimed at countering misinformation. These actions were intended to stem the spread of the disease and protect vulnerable populations.
Effectiveness of Responses and Shortcomings
The effectiveness of these responses varied. While vaccination campaigns helped to increase vaccination rates in some areas, the impact was not uniform across all affected communities. The speed and scale of the response varied depending on the specific location and the level of public health infrastructure. Shortcomings included the persistence of misinformation and the challenges in reaching and convincing hesitant communities.
Summary Table of Factors
| Cause | Impact | Response |
|---|---|---|
| Low vaccination rates | Increased vulnerability to outbreaks; reduced herd immunity; rapid spread within susceptible populations. | Increased vaccination campaigns; targeted outreach to underserved communities; public health education campaigns emphasizing the safety and effectiveness of vaccines. |
| Misinformation and distrust | Reduced vaccine uptake; increased hesitancy; creation of pockets of unvaccinated individuals; difficulty in containing outbreaks. | Fact-checking initiatives; debunking myths and misinformation; community engagement; collaboration with trusted community leaders to build trust in vaccination. |
| Socio-political factors | Disparities in access to healthcare; variations in vaccination rates across socioeconomic groups; community norms affecting vaccination decisions. | Targeted interventions to address health disparities; community outreach programs; addressing underlying social and economic factors affecting vaccination decisions. |
Preventive Measures
The recent measles outbreaks in the Americas underscore the critical need for robust preventive strategies. Effective action requires a multifaceted approach encompassing vaccination campaigns, public health education, and proactive measures to address potential barriers to implementation. A comprehensive strategy will not only reduce the risk of future outbreaks but also strengthen overall public health infrastructure.
Vaccination Strategies and Effectiveness
Measles vaccination remains the cornerstone of prevention. Different vaccination strategies exhibit varying degrees of effectiveness. Universal childhood vaccination programs, coupled with targeted catch-up campaigns for unvaccinated individuals, have proven highly effective in controlling measles outbreaks. Strategies focusing on vulnerable populations, such as those with limited access to healthcare, or those in conflict zones, require tailored approaches to maximize their impact.
These targeted strategies need to consider factors like transportation infrastructure, community trust, and access to healthcare facilities.
Comparison of Preventive Measures
| Preventive Measure | Effectiveness | Potential Challenges |
|---|---|---|
| Increased vaccination campaigns | High, particularly when coupled with robust surveillance and response systems. Studies show a strong correlation between high vaccination coverage and a decline in measles cases. | Building public trust and overcoming vaccine hesitancy, ensuring equitable access to vaccines, especially in marginalized communities, and maintaining accurate and up-to-date vaccination records. |
| Public health education and communication | Medium to high, depending on the quality and comprehensiveness of the message. Effective communication campaigns can improve vaccine uptake and promote health literacy. | Reaching diverse populations with tailored messages, combating misinformation, and ensuring the accuracy and reliability of information disseminated. |
| Strengthening surveillance systems | High, enabling rapid detection and response to outbreaks. Early detection allows for timely interventions to contain the spread of the disease. | Maintaining robust surveillance systems, especially in remote or underserved areas, and ensuring the capacity to quickly identify and isolate cases. |
| Targeted interventions for vulnerable populations | High, ensuring that those at highest risk receive the necessary protection. | Identifying vulnerable populations and tailoring interventions to their specific needs and circumstances. This might involve addressing issues like limited access to healthcare or cultural barriers to vaccination. |
Barriers to Implementing Preventive Measures
Several factors can hinder the implementation of effective preventive measures. Vaccine hesitancy, fueled by misinformation and distrust, can significantly reduce vaccination rates. Disparities in access to healthcare, particularly in underserved communities, can limit the effectiveness of vaccination programs. Challenges in maintaining accurate vaccination records and tracking individuals who may have missed vaccinations also present significant obstacles. Furthermore, building and sustaining public trust in health authorities is essential for successful implementation of any public health initiative.
Public Health Education and Communication
Public health education and communication play a critical role in preventing future measles outbreaks. Clear, accurate, and accessible information about the disease, its transmission, and the importance of vaccination is crucial. Tailoring communication strategies to specific demographics, such as age groups, cultural backgrounds, and socioeconomic strata, enhances the effectiveness of these campaigns. Engaging community leaders and influencers can help disseminate accurate information and foster trust.
Tailoring Public Health Campaigns to Specific Demographics
Public health campaigns should be tailored to resonate with the specific needs and characteristics of different demographic groups. For example, campaigns targeting parents of young children might focus on the safety and efficacy of vaccines. Those targeting adolescents might emphasize the importance of vaccination for their social circles and future health. Community engagement and outreach programs tailored to specific languages and cultural contexts can ensure the message is received and understood effectively.
The message needs to be appropriate and trustworthy for the target audience.
Impact of the Measles Outbreak: Jarvis Americas Measles Outbreak Was Entirely Avoidable
The preventable measles outbreak has had a devastating impact far beyond the initial infections. The long-term health consequences, economic costs, strain on healthcare systems, and psychological toll on affected communities are significant and require careful attention. Understanding these impacts is crucial for developing effective strategies to prevent future outbreaks and support those affected.
Long-Term Health Consequences for Affected Individuals
Measles, though often considered a childhood illness, can have lasting complications. These can range from mild to severe and include encephalitis (inflammation of the brain), pneumonia, and even death. In some cases, individuals experience long-term disabilities like hearing loss, intellectual impairment, or vision problems. The severity of these complications varies greatly depending on factors like age, pre-existing health conditions, and the quality of medical care received.
The Jarvis Americas measles outbreak was truly a tragedy, and completely avoidable. Thankfully, celebrations like a Livermore winemaker winning best white at the SF Chronicle competition here remind us of the joys in life, and highlight the importance of responsible choices in health. It’s a stark reminder that focusing on preventable issues like vaccination saves lives and allows for much more positive news to come out.
Early and prompt medical intervention can often mitigate the long-term damage, but the lasting effects can be profound and impactful on the lives of affected individuals.
Economic Impact of the Measles Outbreak
The economic burden of a measles outbreak extends far beyond direct medical costs. Lost productivity due to illness and subsequent time off work impacts families and businesses. This loss of income can cascade throughout the economy, leading to reduced economic activity and financial strain. Additionally, the cost of public health interventions, including contact tracing and vaccination campaigns, adds to the overall economic burden.
This is exemplified by the significant economic impact of previous outbreaks, where the cost of treatment, lost wages, and public health measures exceeded initial estimations.
Impact on Healthcare Systems and Resources
Measles outbreaks place immense strain on healthcare systems. Hospitals and clinics are overwhelmed by a surge in patients requiring medical attention, leading to longer wait times, increased staff workloads, and potential shortages of essential resources like beds and medical supplies. This strain on resources can impact the ability of healthcare providers to address other health concerns within the community.
Healthcare workers often face significant emotional and physical stress during such outbreaks.
Psychological Toll on Affected Communities, Jarvis americas measles outbreak was entirely avoidable
The fear and anxiety associated with a measles outbreak can have a profound psychological impact on affected communities. Families may experience significant emotional distress due to the illness and the possibility of long-term consequences. The disruption to daily life and the uncertainty surrounding the outbreak can contribute to community-wide anxiety and fear. The collective psychological toll of such an event can persist for some time, necessitating mental health support for those affected.
Examples of Community-Based Support Systems
Community-based support systems play a crucial role in mitigating the impact of an outbreak. These systems can include local organizations providing food assistance, childcare support, and mental health resources. Examples of community-based responses include volunteer organizations assisting families with childcare and providing financial support during times of crisis. This community support is vital in providing essential resources and minimizing the negative effects of the outbreak.
Summary of Impact on Various Sectors
| Sector | Impact |
|---|---|
| Healthcare | Increased workload and resource strain |
| Economy | Reduced productivity and increased costs |
| Education | School closures and disruptions in learning |
| Public Health | Increased surveillance and response efforts |
| Community | Increased anxiety and fear; disruption of daily life |
Public Health Messaging
Effective communication is crucial during public health crises like measles outbreaks. Clear and empathetic messaging can build trust, encourage vaccination, and ultimately curb the spread of disease. Misinformation, unfortunately, often spreads faster than accurate information, making it essential for public health agencies to develop strategies to counter it. This section will explore various approaches to public health communication, focusing on the measles outbreak.Public health messaging must be more than just a collection of facts.
It needs to be tailored to resonate with different communities, build trust, and ultimately inspire action. This requires careful consideration of the target audience, the channels used, and the overall tone of the message. The goal is not just to inform but to motivate individuals to protect themselves and their communities.
The Jarvis America measles outbreak was a tragedy, entirely preventable. It’s a stark reminder of the importance of vaccination. Meanwhile, the Biden administration’s decision to forgive student loan debt for students of the former San Diego-based Ashford University ( biden admin to forgive debt for students of former san diego based ashford university ) highlights a different, yet equally significant, kind of societal responsibility.
Ultimately, both issues point to areas where better planning and proactive measures could have avoided significant hardship.
Different Approaches to Communicating Public Health Information
Effective public health communication employs a variety of approaches, including targeted messaging, community engagement, and utilizing trusted messengers. These methods aim to reach different demographics and build a comprehensive strategy. Clear and concise communication is key.
Examples of Clear and Concise Vaccination Messaging
Clear and concise messaging is vital for encouraging vaccination. Here are some examples:
- “Measles is preventable. Get vaccinated. Protect yourself and your community.” This message is straightforward, highlighting the preventative aspect and the community benefit.
- “Vaccination is safe and effective. Protect your children from measles.” This message emphasizes safety and the importance of protecting children, a crucial demographic.
- “Measles vaccination is the best defense against outbreaks. Get your shots.” This message emphasizes the protective role of vaccination and encourages direct action.
Strategies to Counter Misinformation
Countering misinformation is crucial. It’s not enough just to present the facts; you must actively address the concerns and anxieties driving the spread of false information. Effective strategies include:
- Fact-checking and debunking myths. Identifying and addressing false claims promptly is vital. Public health agencies should maintain active social media presence to counter false information quickly and directly.
- Collaborating with trusted community leaders. Using local leaders who have credibility within their communities can significantly enhance the effectiveness of public health messaging. This builds trust and fosters a sense of shared responsibility.
- Using multiple communication channels. Reaching diverse audiences requires utilizing a variety of platforms, including social media, local media, and community events.
Tailoring Messaging to Different Demographics
Effective public health messaging considers the needs and perspectives of different demographics. For example, messaging aimed at parents might emphasize the safety and effectiveness of vaccines, while messaging aimed at adolescents might focus on the importance of protecting their peers and friends. Public health agencies must tailor their messaging to address the specific concerns of different communities.
Best Practices in Public Health Communication
Best practices include:
- Transparency and honesty. Open communication builds trust and allows individuals to understand the situation.
- Empathy and understanding. Public health messages should be crafted with compassion and address concerns with sensitivity.
- Consistency and repetition. Regular reminders and reinforcement of key messages are crucial.
Importance of Transparency and Trust in Public Health Messaging
Transparency and trust are fundamental to successful public health messaging. Openly sharing information, acknowledging uncertainties, and responding to concerns with honesty fosters trust. This approach allows communities to feel empowered and involved in the response.
Creating a Visually Appealing Infographic
An infographic summarizing the measles outbreak should be visually appealing and easy to understand. Key elements might include:
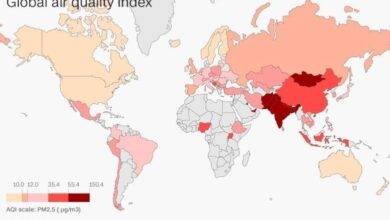
- Clear and concise data visualization. Charts and graphs effectively illustrate key statistics, such as the number of cases, location, and age groups affected.
- Engaging visuals. Images and icons can help convey complex information in an easily digestible format.
- Simple language. Avoid jargon and use plain language that is accessible to all audiences.
International Cooperation
The recent measles outbreaks underscore the critical need for international cooperation in public health. Global interconnectedness means that a health crisis in one country can rapidly spread to others, highlighting the shared responsibility for preventing and responding to such outbreaks. Effective responses demand a coordinated global effort, leveraging expertise and resources across borders.International organizations play a crucial role in fostering this cooperation, acting as a central hub for knowledge sharing, resource allocation, and standardized protocols.
Their interventions are essential for building resilience to future outbreaks and ensuring a safer, healthier world for all.
The Role of International Organizations
International organizations, particularly the World Health Organization (WHO), are vital in coordinating global responses to outbreaks like measles. They establish global standards for disease surveillance, vaccination campaigns, and public health messaging. This coordinated approach ensures that best practices are shared and implemented across nations, minimizing the spread of disease and mitigating the impact of outbreaks. The WHO, for example, provides technical guidance and support to countries facing outbreaks, facilitating the sharing of data and best practices.
Global Cooperation in Public Health
Global cooperation is paramount for effective public health. A unified front allows for the rapid mobilization of resources and expertise, enabling swift and coordinated responses to emerging health threats. This collaborative approach fosters trust and shared responsibility, empowering countries to work together to overcome challenges. Sharing data and best practices ensures that lessons learned from one outbreak can be applied to prevent similar outbreaks in other regions.
Comparative Approaches to Outbreak Response
Different countries employ varying approaches to responding to outbreaks. Some prioritize rapid vaccination campaigns, while others focus on enhanced surveillance and contact tracing. The specific strategies often depend on factors such as the country’s healthcare infrastructure, vaccination rates, and the severity of the outbreak. Understanding and comparing these approaches allows for a more nuanced understanding of effective strategies in diverse contexts.
For instance, countries with robust healthcare systems might have more capacity to conduct extensive contact tracing, while countries with lower vaccination rates might prioritize mass vaccination campaigns.
Examples of Successful International Collaborations
Numerous examples demonstrate the success of international collaborations in containing outbreaks. The global eradication of smallpox is a prime example of what can be achieved through concerted international efforts, leveraging resources and expertise across borders. The response to the recent Ebola outbreaks also showcased the importance of international partnerships in coordinating aid and support. These collaborations are crucial for ensuring timely interventions and effective containment.
Importance of Sharing Data and Best Practices
Sharing data and best practices is essential for preventing future outbreaks. This exchange of information allows countries to learn from each other’s experiences, identifying successful strategies and mitigating potential failures. Open communication fosters a culture of learning and adaptation, enabling better responses to future health crises. For instance, if one country develops a particularly effective contact tracing app, sharing this information with other countries can accelerate their own response strategies.
Key Players in International Response
| Organization | Role |
|---|---|
| WHO | Coordinating global efforts, providing technical guidance, and promoting best practices. |
| UNICEF | Supporting vaccination campaigns, especially in underserved populations. |
| Global Fund to Fight AIDS, Tuberculosis and Malaria | Funding and supporting efforts to strengthen health systems and address underlying factors that increase vulnerability. |
| Other international organizations (e.g., the World Bank) | Providing financial and technical assistance for strengthening healthcare infrastructure and response capacity. |
Closure
In conclusion, the Jarvis Americas measles outbreak serves as a stark reminder of the importance of vaccination and robust public health measures. Preventing future outbreaks requires a multifaceted approach that addresses the underlying causes, strengthens public health infrastructure, and promotes accurate information. This necessitates a collaborative effort between governments, healthcare professionals, and communities, fostering trust and transparency to ensure that misinformation does not undermine public health initiatives.
International cooperation is also crucial, sharing data and best practices to safeguard global health.