Treatment Test Failures Patient Protection
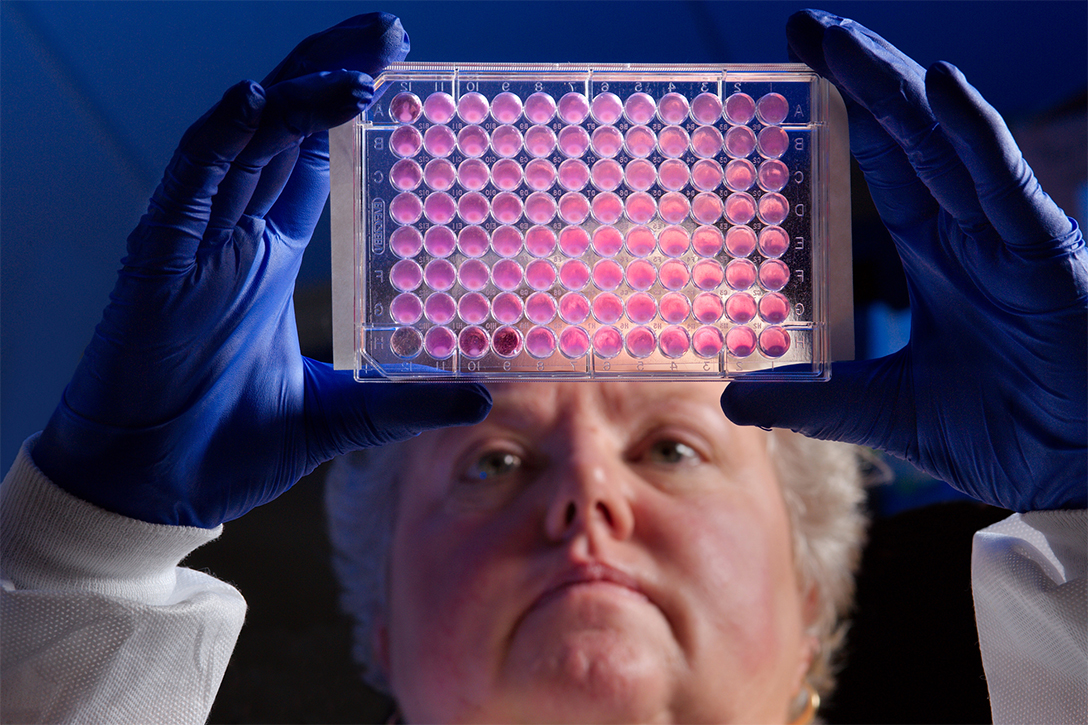
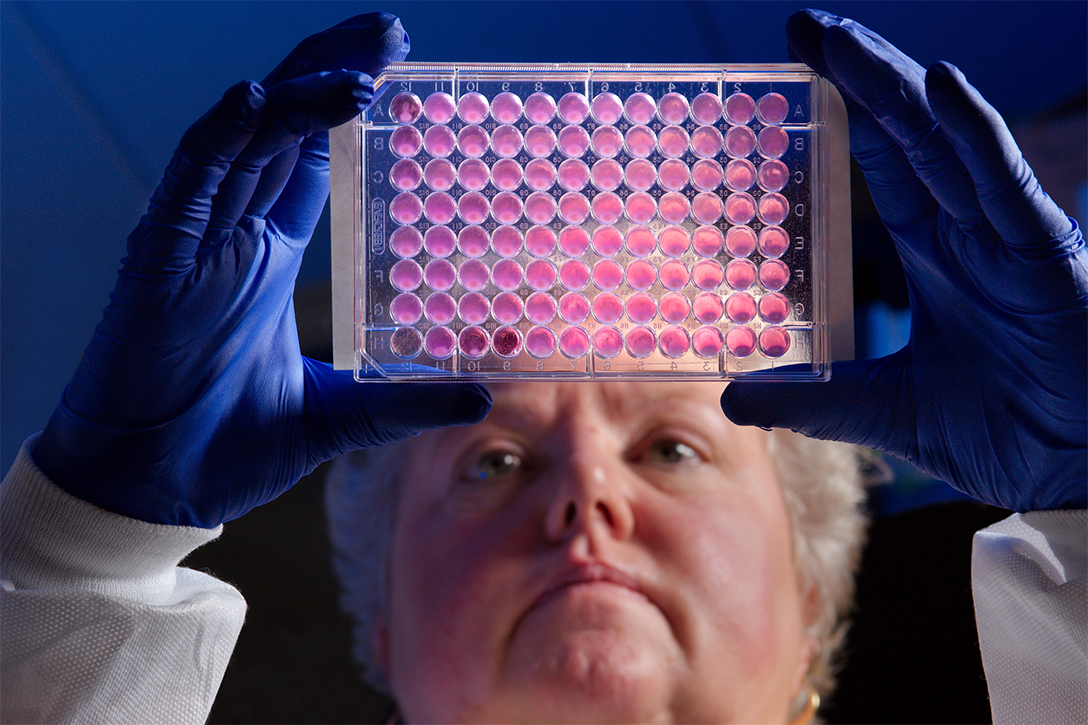
They said it failing to protect patients in treatment test. This article delves into the critical issue of patient safety in clinical trials, examining the causes, consequences, and systemic factors contributing to treatment test failures. We’ll explore how failures can impact participants, erode public trust, and necessitate significant changes in the research process.
From inadequate safety protocols to flaws in design and execution, various factors contribute to these failures. Understanding these elements is crucial for creating more robust and ethical treatment testing methodologies that prioritize patient well-being.
Defining the Treatment Test Failure

A treatment test failure to protect patients is a serious event where the procedures or protocols designed to safeguard participants during the course of a clinical trial prove inadequate. This inadequacy can lead to harm or prevent the trial from achieving its intended outcomes. Understanding the various facets of a treatment test failure is crucial for identifying areas needing improvement and strengthening future trials.A treatment test failure to protect patients encompasses a wide range of potential shortcomings.
These failures can range from protocol violations to unforeseen adverse events, and their impact can vary greatly depending on the severity and frequency of the failures. Recognizing these diverse types of failures is essential for developing robust preventative measures.
Types of Treatment Test Failures
Treatment test failures can manifest in several ways. These failures can stem from issues in design, execution, or monitoring of the trial.
- Protocol Violations: This involves deviations from the predefined study protocol. Examples include incorrect dosage administration, inappropriate patient selection criteria, or failure to adhere to established safety procedures. These can stem from human error, inadequate training, or systemic issues within the research team.
- Unforeseen Adverse Events: Unexpected side effects or complications arising from the treatment under investigation can pose risks to participants. These can range from mild discomfort to severe, life-threatening conditions. Examples include allergic reactions, organ damage, or psychological distress. The severity and frequency of these events are crucial indicators of the test’s effectiveness in protecting patients.
- Inadequate Monitoring: Failure to adequately monitor patients for adverse effects during the trial is another potential failure point. This can include insufficient frequency of checkups, lack of vigilance in recording observations, or failure to promptly address concerns. This can lead to missed opportunities to intervene and prevent further harm.
- Insufficient Risk Assessment: Before initiating a treatment test, a comprehensive risk assessment should be performed. A failure in this stage involves overlooking potential risks, or an underestimation of the risk factors. A failure to anticipate and adequately address potential risks can compromise the safety of participants. Examples include insufficient data on the treatment’s potential long-term effects or insufficient understanding of the patient population’s baseline characteristics.
Examples of Treatment Test Failures
Several historical examples highlight the importance of stringent safety measures in treatment tests.
- Thalidomide tragedy: This infamous case underscores the necessity for rigorous pre-market testing. The drug, initially approved for use, caused severe birth defects in children born to mothers who took the drug during pregnancy. The lack of sufficient testing in this case resulted in widespread harm and significant regulatory changes.
- Early testing of a new cancer drug: A test that fails to adequately monitor patients for the occurrence of rare but potentially severe side effects, such as severe bleeding, may lead to adverse outcomes for participants. This underscores the need for close monitoring and reporting procedures.
Stages of Treatment Test Failures
Treatment test failures can occur at various stages of the trial.
- Pre-clinical phase: Failures in the pre-clinical phase may involve inadequate testing of the treatment on animal models or failure to identify potential toxicity risks. This can result in unforeseen issues during human trials.
- Phase I: In this phase, the focus is on safety and dosage. Failures here might include insufficient testing of different doses or a lack of appropriate safety monitoring protocols.
- Phase II and III: These phases involve expanding the test population and evaluating efficacy. Failures here might include inadequate participant selection, leading to the wrong patient population being tested, or insufficient blinding in the testing process.
- Post-marketing surveillance: Even after a treatment is approved, monitoring is critical. Failures here involve inadequate tracking of long-term effects after the treatment is released to the public. This can reveal unforeseen problems that were not apparent during initial trials.
Key Factors Contributing to Treatment Test Failures
Several factors contribute to a treatment test failing to protect patients.
- Insufficient funding: Limited resources can lead to inadequate staffing, poor infrastructure, or a lack of advanced equipment, hindering proper safety monitoring and analysis.
- Inadequate oversight: Lack of robust regulatory oversight or weak internal review processes can allow issues to persist without being addressed.
- Lack of clear communication: Poor communication between researchers, participants, and regulatory bodies can lead to missed opportunities for early intervention and the reporting of critical information.
- Human error: Oversights or mistakes made by individuals involved in the trial can compromise the safety of participants. This can include errors in data entry, incorrect dosage administration, or poor adherence to safety procedures.
Causes of Patient Protection Failure: They Said It Failing To Protect Patients In Treatment Test
Treatment tests, designed to evaluate new therapies, hold immense promise for improving patient outcomes. However, failures in patient protection during these trials can have severe consequences, potentially leading to harm or even death. Understanding the root causes of these failures is crucial for strengthening safety protocols and ensuring the ethical conduct of future research.Identifying and addressing the underlying factors behind treatment test failures is essential for improving patient safety and the integrity of medical research.
A multifaceted approach is needed, encompassing rigorous safety protocols, meticulous risk assessments, and careful scrutiny of trial design and execution.
The recent criticism of the treatment test for failing to protect patients is concerning. It’s a critical issue, especially when considering the importance of patient safety. To stay focused and organized while reviewing complex data like this, a good portable computer monitor like the best portable computer monitor can really help. Ultimately, the test’s shortcomings need thorough investigation to ensure patient well-being in future trials.
Inadequate Safety Protocols
Safety protocols are the bedrock of any treatment test. Their effectiveness directly impacts patient safety. Insufficient protocols can leave patients vulnerable to unforeseen risks. This includes lacking clear procedures for monitoring adverse events, inadequate training for research staff, and insufficient provisions for emergency response. Failing to anticipate and address potential complications is a significant risk factor.
For example, a trial lacking detailed procedures for managing allergic reactions could lead to severe consequences for participants.
Poor Risk Assessment
Comprehensive risk assessment is vital for identifying potential dangers associated with a new treatment. A flawed risk assessment may underestimate or entirely overlook possible adverse effects. This can lead to the enrollment of patients who are particularly vulnerable to the risks associated with the treatment. Incomplete or inaccurate data on the treatment’s potential side effects, or neglecting to consider the interplay of pre-existing conditions with the treatment, can be crucial flaws.
For instance, a trial that fails to adequately assess the risk of drug interactions for patients taking multiple medications could expose participants to unexpected and dangerous complications.
Flaws in Treatment Test Design and Execution
The design and execution of treatment tests can introduce vulnerabilities that compromise patient safety. Insufficient blinding procedures can introduce bias, leading to inaccurate conclusions about treatment effectiveness and potential harm. Poorly defined inclusion and exclusion criteria may result in enrolling patients who are not suitable for the treatment, increasing the risk of adverse outcomes. Inadequate data collection methods or analysis can lead to misinterpretations of the treatment’s effects, masking potentially dangerous side effects.
For example, if a trial fails to account for the impact of lifestyle factors on the treatment, it could misrepresent the true risk profile for different subgroups of participants.
Comparison of Patient Safety Approaches
Different approaches to patient safety in treatment tests exist, each with its strengths and weaknesses. Some focus on pre-emptive measures, such as rigorous safety protocols and thorough risk assessments. Others emphasize proactive monitoring, such as frequent assessments of participants for adverse events and quick response mechanisms. An effective approach integrates both strategies, ensuring a comprehensive safety net for participants.
Comparing these approaches can reveal areas for improvement in existing procedures.
Potential Flaws in Treatment Test Design and Execution
Several potential flaws can compromise patient safety in treatment tests. These include: inadequate blinding procedures, inappropriate selection of participants based on poor inclusion/exclusion criteria, insufficient monitoring of adverse events, lack of clear emergency response plans, and insufficient data analysis. The impact of these flaws can be severe, leading to unnecessary patient harm or even fatalities.
Consequences of Failure
Treatment test failures, while rare, can have devastating consequences for patients, researchers, and the public’s trust in medical advancements. These failures often lead to serious harm, erode public confidence in research, and trigger complex legal and ethical issues. Understanding these consequences is crucial for improving future trials and safeguarding patient well-being.The failure of a treatment test to protect patients during clinical trials can have far-reaching repercussions.
These repercussions extend beyond the immediate trial participants, affecting the broader medical community and public perception of scientific research. Proper protocols and oversight are essential to prevent such failures and ensure the safety and well-being of all participants.
Potential Harm to Participants
Treatment test failures can result in various forms of harm to participants. These harms can range from minor discomfort to severe adverse effects, potentially leading to long-term health issues or even death. Examples include allergic reactions, infections, organ damage, and psychological distress. Careful monitoring and risk assessment are vital to minimize the likelihood of harm.
Impact on Public Trust in Medical Research
Failures in treatment tests can severely damage public trust in medical research. When research is compromised or fails to protect participants, the public may lose confidence in the integrity of scientific endeavors. This loss of trust can hinder the development of new treatments and therapies, impacting the lives of countless individuals. Building and maintaining public trust is paramount for fostering collaboration and acceptance of medical advancements.
Legal and Ethical Implications
Treatment test failures have significant legal and ethical ramifications. Researchers and institutions involved in such failures may face legal action from affected participants. Ethical breaches, such as inadequate informed consent procedures or insufficient safety measures, can lead to investigations and sanctions. Strict adherence to ethical guidelines and regulations is crucial to avoid such legal and ethical conflicts.
They said it was failing to protect patients in treatment tests, a serious concern. Meanwhile, the latest treasury secretary says Trump will keep the 10% import tariff raise on Chinese goods, potentially impacting global trade and the very research that needs better patient protections. This whole situation highlights the complex interplay between economic policies and healthcare advancements.
Procedures for Handling Treatment Test Failures
When a treatment test fails to protect patients, transparent and comprehensive procedures are essential to address the issue. This includes immediate reporting of any adverse events, thorough investigation into the causes of the failure, and implementation of corrective actions to prevent similar occurrences in the future. The establishment of clear protocols for handling failures is essential to maintain patient safety and integrity within medical research.
A robust system of oversight and reporting is critical. An independent review of the failed trial is usually conducted to determine the exact causes of the failure and implement preventative measures.
Systemic Issues and Recommendations
Treatment tests, crucial for evaluating new therapies, demand meticulous safety protocols. Failures in these tests can have severe consequences for patients, leading to harm or even death. Addressing systemic issues within the design, execution, and oversight of these trials is paramount to ensuring patient safety and the integrity of the research process. This section delves into a framework for evaluating safety, identifies systemic problems, and proposes actionable recommendations for improvement.A comprehensive approach is needed to move beyond reactive problem-solving and instead create a proactive system for safeguarding patients in treatment tests.
This involves establishing clear standards, robust monitoring mechanisms, and transparent communication channels. This section details a structured approach to these crucial aspects.
Framework for Evaluating Overall Safety of Treatment Tests
A robust framework for evaluating the overall safety of treatment tests necessitates a multi-faceted approach. This framework should encompass pre-test assessments of risk factors, ongoing monitoring of patient well-being, and post-test analyses of outcomes. The framework should be designed to identify potential risks early in the process and to adapt to emerging data and concerns. It must also facilitate transparent communication among researchers, clinicians, and regulatory bodies.
Identifying Systemic Issues Contributing to Treatment Test Failures
Several systemic issues contribute to treatment test failures. These include inadequate risk assessment, insufficient patient monitoring, lack of clear reporting mechanisms, and inadequate training for researchers and clinical staff. Furthermore, inadequate resources and regulatory oversight can hinder the successful execution and evaluation of treatment tests. Poor communication between research teams, ethics committees, and regulatory bodies also poses a significant systemic issue.
Recommendations for Improving Patient Protection in Treatment Tests
Implementing improvements in patient protection requires a multi-pronged strategy. Recommendations include enhanced risk assessments, proactive monitoring, improved data collection and analysis, and rigorous reporting procedures.
- Strengthened Risk Assessment Protocols: A thorough pre-test risk assessment should be mandatory, considering potential adverse effects, patient demographics, and baseline health conditions. This assessment should involve input from multiple experts and be reviewed and updated regularly.
- Enhanced Patient Monitoring: Establish standardized and frequent monitoring procedures for patients throughout the test, including vital signs, symptom reporting, and adverse event tracking. Real-time data analysis should be incorporated into the monitoring process.
- Robust Data Collection and Analysis: Implement rigorous data collection protocols and establish clear guidelines for data analysis. This includes ensuring data integrity, privacy, and confidentiality.
- Improved Reporting Procedures: Establish clear and transparent reporting procedures for adverse events and other safety concerns. Develop a system that allows for rapid escalation and appropriate responses to serious events.
- Comprehensive Training: Provide comprehensive training to researchers, clinicians, and support staff on ethical conduct, safety procedures, and data management. Regular updates and refresher courses are crucial.
Reviewing and Updating Treatment Test Protocols
Regular review and updating of treatment test protocols are essential to maintaining safety and effectiveness. This process should involve input from diverse stakeholders, including researchers, clinicians, patients, and regulatory bodies. A structured process should be in place to address emerging data, evolving best practices, and new safety concerns.
Summary Table: Common Systemic Issues and Potential Solutions
| Issue | Potential Solution | Impact | Evaluation Method |
|---|---|---|---|
| Inadequate risk assessment | Develop standardized risk assessment tools and protocols; include input from diverse experts. | Reduced risk of harm; improved accuracy of predictions | Compare pre-test risk assessment scores with post-test outcomes. |
| Insufficient patient monitoring | Implement standardized, frequent monitoring protocols; use real-time data analysis tools. | Early detection of adverse events; quicker response to safety concerns | Track frequency and timeliness of patient monitoring records. |
| Lack of clear reporting mechanisms | Establish clear, standardized reporting protocols for adverse events; facilitate rapid escalation to appropriate authorities. | Increased transparency and accountability; quicker response to serious issues | Analyze reporting frequency and timeliness of action taken in response to reported events. |
Illustrative Case Studies
Unveiling the dark side of treatment test failures requires a careful examination of real-world examples. These case studies serve as crucial learning opportunities, highlighting the vulnerabilities within the system and the devastating consequences for patients. They illuminate the intricate web of factors contributing to these failures, from flawed protocols to inadequate oversight. Analyzing these past mistakes is paramount for crafting a more robust and patient-centered future.
Case Study 1: The Thalidomide Tragedy, They said it failing to protect patients in treatment test
The thalidomide tragedy of the 1960s stands as a stark reminder of the potential for catastrophic consequences when rigorous testing and safety protocols are ignored. Thalidomide, initially marketed as a sedative and anti-nausea medication, was prescribed widely. However, it later emerged that the drug caused severe birth defects in infants born to mothers who took it during pregnancy.
This widespread harm resulted from a lack of adequate pre-market testing for potential teratogenic effects. The failure to identify the drug’s detrimental impact on developing fetuses exposed a critical flaw in the pharmaceutical testing process. The lessons learned from this tragedy are profound: meticulous testing, rigorous scrutiny of potential side effects, and a heightened awareness of the unique vulnerabilities of pregnant women are paramount.
Case Study 2: The Vioxx Controversy
The withdrawal of Vioxx, a popular nonsteroidal anti-inflammatory drug (NSAID), exemplifies a different type of treatment test failure. While initially marketed as a safer alternative to other NSAIDs, long-term studies revealed an increased risk of heart attack and stroke in patients taking Vioxx. This failure stemmed from a combination of factors, including inadequate consideration of long-term cardiovascular risks and a prioritization of short-term efficacy over long-term safety.
The case underscored the need for robust and sustained long-term follow-up studies in clinical trials, focusing on potential side effects beyond the initial phase of the trial.
Case Study 3: The Early COVID-19 Vaccine Trials
The initial stages of COVID-19 vaccine development highlighted the complexity of clinical trial design and the importance of ethical considerations. Several early vaccine trials faced challenges in accurately measuring efficacy, particularly with the rapid and evolving nature of the pandemic. This led to some concerns about the rigor of the trials and the potential for overlooking long-term effects.
The rapid development of the vaccines, while essential, also led to a compressed timeframe for testing, potentially compromising the thoroughness of long-term safety assessments. The case underlines the need for robust, transparent data collection and analysis throughout the vaccine development process, even during a pandemic.
So, they’re saying the treatment trial failed to adequately protect patients. It’s a serious issue, and while watching Trump’s speech to Congress Tuesday might seem unrelated, this is a good resource for finding out how to watch it, it does highlight the need for transparency and rigorous testing in these kinds of situations. Hopefully, the scrutiny will push for improvements in patient safety during future trials.
Comparison of Case Studies
| Case Study | Patient Harm | Root Cause | Lessons Learned |
|---|---|---|---|
| Thalidomide Tragedy | Severe birth defects | Lack of adequate pre-market testing for teratogenic effects | Rigorous testing, scrutiny of potential side effects, and heightened awareness of vulnerable populations. |
| Vioxx Controversy | Increased risk of heart attack and stroke | Inadequate long-term cardiovascular risk assessment | Robust and sustained long-term follow-up studies in clinical trials. |
| Early COVID-19 Vaccine Trials | Potential for overlooking long-term effects | Challenges in accurately measuring efficacy and potential limitations of rapid development | Robust, transparent data collection and analysis throughout the vaccine development process, even during a pandemic. |
Future Considerations
Looking ahead, safeguarding patient well-being in treatment trials necessitates proactive measures to anticipate and address potential challenges. Technological advancements, while promising, also introduce new complexities that must be carefully navigated. Proactive strategies and a commitment to continuous improvement are crucial for ensuring the safety and ethical conduct of future clinical trials.
Emerging Challenges to Patient Protection
The evolving landscape of healthcare presents novel challenges to patient protection in treatment trials. These include the increasing complexity of trial designs, the emergence of novel therapies with unpredictable side effects, and the potential for biases in data collection and analysis. The growing reliance on remote monitoring and digital technologies, while offering opportunities for enhanced patient engagement and data capture, also raises concerns about data security, privacy, and equitable access.
Furthermore, the potential for misinterpretation of complex data from these technologies necessitates robust validation and quality control measures.
Technological Advancements and Patient Safety
Technological advancements, such as artificial intelligence (AI) and machine learning (ML), hold significant promise for enhancing patient safety in clinical trials. AI can be employed to identify patterns in patient data that might indicate emerging risks or adverse events, allowing for early intervention and mitigation. Real-time monitoring systems, leveraging wearable technology and remote sensing, can provide continuous data streams about patients’ physiological and behavioral responses to treatments, enabling quicker responses to potential safety concerns.
However, the implementation of these technologies requires careful consideration of data privacy, security, and the potential for algorithmic bias.
New Strategies for Preventing Future Failures
To mitigate future patient protection failures, a multi-faceted approach is needed. This includes fostering a culture of safety within clinical trial organizations, establishing robust regulatory frameworks that adapt to technological advancements, and investing in training and education for researchers and clinicians. Transparent communication protocols are essential for disseminating information about emerging risks and adverse events to relevant stakeholders.
Furthermore, independent audits and quality control measures should be implemented to ensure data integrity and adherence to ethical guidelines.
Illustrative Examples of Emerging Research in Patient Safety
Several research initiatives are actively exploring innovative approaches to patient safety in clinical trials. For instance, studies are examining the use of predictive modeling to identify patients at higher risk of adverse events. Other research focuses on developing novel algorithms to analyze large datasets of patient data in real-time to detect subtle patterns indicative of emerging safety concerns.
These efforts demonstrate the potential for technology to enhance the safety of clinical trials.
Evolving Role of Technology in Patient Protection
| Technology | Application | Potential Impact |
|---|---|---|
| Artificial Intelligence (AI) | Predictive modeling of adverse events, real-time data analysis | Early identification of safety risks, proactive interventions |
| Machine Learning (ML) | Pattern recognition in patient data, risk stratification | Improved risk assessment, targeted interventions |
| Wearable Sensors | Continuous physiological monitoring, remote patient data collection | Enhanced surveillance, faster responses to adverse events |
| Remote Monitoring Systems | Real-time tracking of vital signs, behavioral data | Early detection of potential safety concerns, reduced hospitalizations |
Final Review
In conclusion, ensuring patient protection in treatment tests requires a multifaceted approach that considers both immediate safeguards and long-term systemic improvements. By learning from past failures, adapting to technological advancements, and fostering a culture of safety, we can strive for more reliable and ethical clinical trials that benefit both participants and the wider medical community. This discussion underscores the importance of continuous evaluation and improvement in research protocols to maintain public trust and uphold the highest ethical standards.