Texas Measles Surge National Threat
Measles exploded in texas after stagnant vaccine funding new cuts threaten the same across the us – Measles exploded in Texas after stagnant vaccine funding. New cuts threaten the same across the US. This alarming situation highlights a critical public health concern, demonstrating the direct link between underfunded vaccination programs and rising rates of preventable diseases. The recent surge in Texas serves as a stark warning, raising concerns about the potential for similar outbreaks across the nation.
We’ll delve into the specific factors contributing to this crisis, examine the impact of stagnant funding, and explore potential strategies for prevention.
This situation underscores the urgent need for increased funding and proactive public health measures. The article examines the correlation between declining vaccine funding and the resurgence of measles, offering insights into the crisis’s implications for public health and the economy. The report also examines the role of misinformation and hesitancy in impacting vaccination rates, along with the importance of community engagement in addressing this public health crisis.
Measles Outbreak in Texas
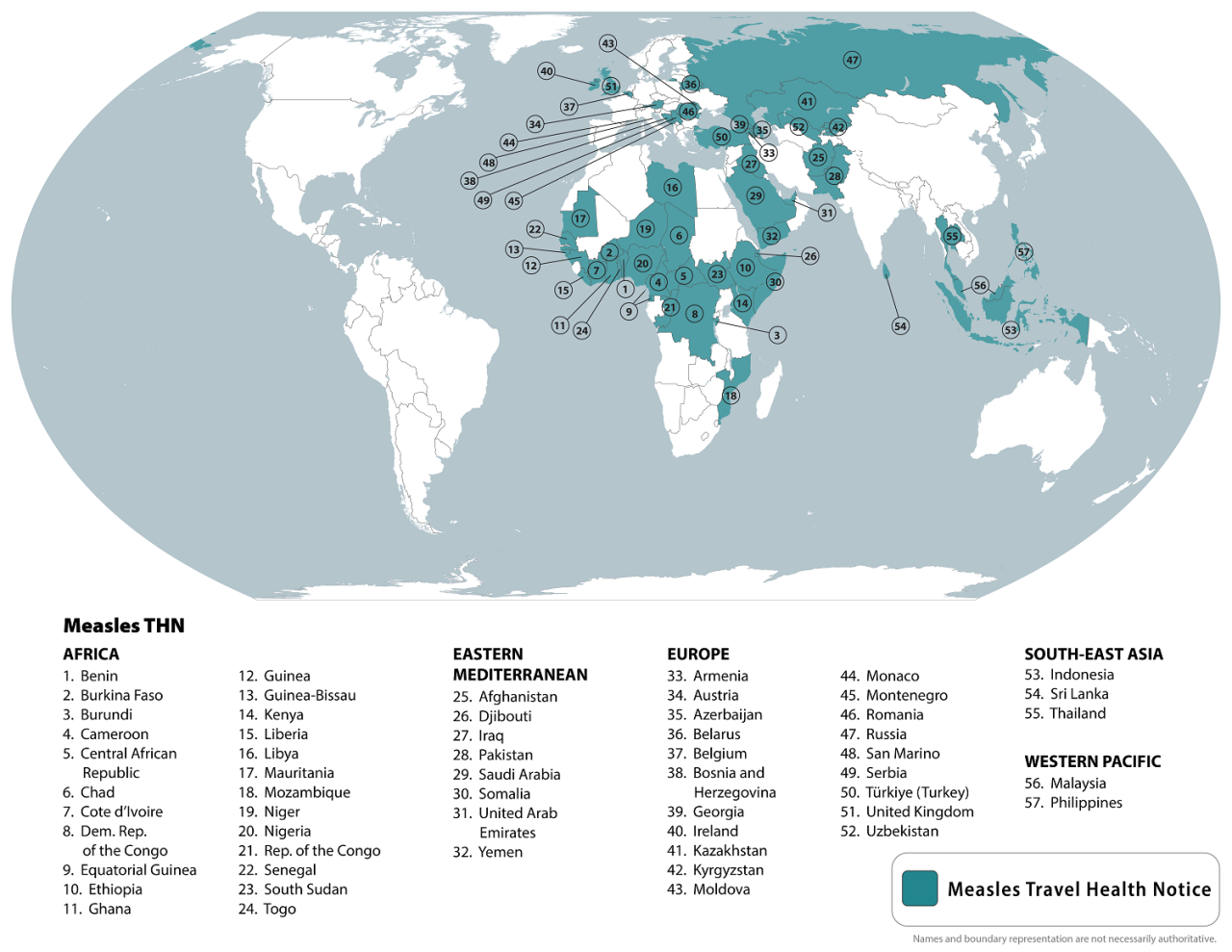
The recent surge in measles cases in Texas serves as a stark reminder of the importance of vaccination. While measles had been largely contained in the US, this resurgence highlights vulnerabilities in public health infrastructure and the potential for outbreaks to rapidly escalate, particularly when vaccination rates decline. This situation underscores the need for proactive measures to prevent future outbreaks and emphasizes the critical link between funding and public health outcomes.The correlation between stagnant vaccine funding and the recent measles surge in Texas is undeniable.
Reduced funding for public health initiatives often leads to decreased capacity for disease surveillance, contact tracing, and community outreach, all essential components in controlling the spread of infectious diseases. Insufficient resources hinder the ability to effectively identify and contain outbreaks, leading to a wider reach of the virus. These issues are not unique to Texas; similar patterns have been observed in other states and countries.
The measles outbreak in Texas, fueled by stagnant vaccine funding, is a serious concern. New cuts threaten similar outbreaks across the US. This alarming trend highlights the critical need for consistent funding and awareness campaigns. For example, Joseph Schaefers, a prominent figure in Cupertino, CA, joseph schaefers cupertino ca has been advocating for community health initiatives.
Ultimately, preventative measures and sustained funding are crucial to combatting the spread of preventable illnesses like measles.
Historical Context of Measles Outbreaks in Texas
Measles outbreaks have occurred periodically throughout Texas’ history, often coinciding with periods of low vaccination rates. Factors such as socioeconomic disparities, access to healthcare, and misinformation campaigns regarding vaccines have contributed to these fluctuations. Analyzing historical data reveals patterns in the demographics most affected, which can guide targeted interventions.
Correlation Between Stagnant Vaccine Funding and the Recent Measles Surge, Measles exploded in texas after stagnant vaccine funding new cuts threaten the same across the us
The recent measles surge in Texas is intricately linked to stagnant vaccine funding. Decreased resources have resulted in a weakened public health infrastructure, impacting the ability to effectively monitor and respond to outbreaks. This has created a breeding ground for the virus to spread more rapidly.
Strategies Employed by Texas Health Officials to Combat the Outbreak
Texas health officials have implemented various strategies to combat the measles outbreak, including intensified surveillance, contact tracing, and public health campaigns. These initiatives aim to identify infected individuals, isolate them, and educate the public about the importance of vaccination. Effective communication plays a crucial role in these efforts.
Successful Interventions in Similar Outbreaks in Other States or Countries
Several states and countries have successfully contained similar measles outbreaks through comprehensive public health interventions. These strategies often include targeted vaccination campaigns, particularly in communities with lower vaccination rates, and public awareness campaigns emphasizing the safety and effectiveness of vaccines.
Comparison of the Current Texas Outbreak to Previous Outbreaks
| Characteristic | Current Outbreak | Previous Outbreak (Example) |
|---|---|---|
| Affected Demographics | Predominantly children and young adults, with some reports of individuals with compromised immune systems | Similar demographics, but with potential variations depending on the specific factors of each outbreak |
| Vaccination Rates | Data from Texas Department of State Health Services indicates lower vaccination rates in certain areas | Historical data may show lower vaccination rates in the affected regions during the prior outbreak |
| Severity | Moderate severity, with a substantial number of reported cases | Severity can vary depending on the factors influencing the outbreak |
Vaccination Programs Available in Texas and Their Accessibility
The availability and accessibility of vaccination programs vary across Texas. This table highlights different vaccination programs available and their accessibility to various populations:
| Vaccination Program | Target Population | Accessibility |
|---|---|---|
| Texas Vaccines for Children Program | Children under 19 years old, uninsured, or underinsured | Generally accessible through participating healthcare providers |
| Free Clinics | Low-income and uninsured individuals | Varying accessibility depending on location and availability |
| Public Health Clinics | General population, including vulnerable populations | Accessible through local health departments |
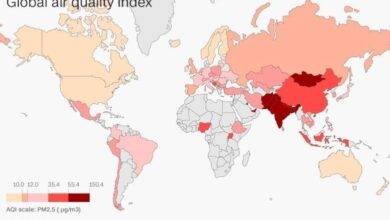
National Implications of Vaccine Funding Cuts
The recent measles outbreak in Texas, tragically exacerbated by stagnant vaccine funding, serves as a stark reminder of the national implications of underinvesting in public health initiatives. This isn’t an isolated incident; similar trends are emerging across the US, with potential repercussions for the entire nation’s public health infrastructure. The interconnected nature of our communities means that a health crisis in one area can quickly become a national problem if not addressed proactively.The issue is multifaceted.
Funding cuts to vaccination programs directly impact the availability of vaccines, potentially hindering access for vulnerable populations. Furthermore, reduced resources for disease surveillance and outbreak response create significant challenges in containing future outbreaks and tracking the spread of infectious diseases. This creates a ripple effect, threatening the hard-won progress in disease prevention and control.
Broader Implications on Vaccination Rates
Decreased funding for vaccination programs often leads to a decline in vaccination rates. This can be attributed to several factors, including reduced access to vaccines, diminished public health outreach, and less availability of vaccination clinics. Consequently, communities with lower vaccination rates become more susceptible to outbreaks of vaccine-preventable diseases. This is particularly true for vulnerable populations who may face additional barriers to accessing healthcare.
Potential Consequences for Public Health
The consequences of reduced vaccine funding extend beyond measles. A decrease in vaccination rates increases the risk of other vaccine-preventable diseases, such as mumps, rubella, polio, and whooping cough. These diseases, once largely controlled, could experience resurgence, leading to substantial public health crises. The resurgence of preventable diseases would strain healthcare systems and impact individuals and families. The ripple effect would impact not just physical health, but also the mental and emotional well-being of those affected.
The measles outbreak in Texas, fueled by stagnant vaccine funding, is a serious concern, and new cuts risk similar outbreaks nationwide. Thankfully, local communities are stepping up to address the issue. For example, Marin County is considering a $5.2 million loan to support a Habitat for Humanity housing project, highlighting a broader effort to improve community well-being, which is crucial in the face of potential public health crises.
This kind of proactive approach, coupled with robust vaccine funding, is vital to prevent future measles outbreaks. marin county considering 5 2 million loan for habitat for humanity housing project Ultimately, the lack of vaccine funding threatens the health of our communities, highlighting the importance of addressing these issues comprehensively.
Comparison of Vaccination Rates and Funding Levels
Comparing vaccination rates across different states with varying funding levels can highlight the correlation. States with lower funding for vaccination programs often exhibit lower vaccination rates, creating a higher risk of outbreaks. For example, a state with substantial funding might maintain high vaccination rates, offering a protective barrier against the spread of diseases. Conversely, states with inadequate funding might experience a greater vulnerability to outbreaks.
A comprehensive analysis comparing vaccination rates and corresponding funding levels in various states would provide a clearer picture of this relationship.
Economic Burden of Measles Outbreaks
Measles outbreaks impose a significant economic burden on healthcare systems. The cost of treating infected individuals, managing outbreaks, and implementing public health measures is substantial. This cost includes hospitalizations, physician visits, lost productivity due to illness, and the strain on healthcare workers. The economic impact extends beyond direct healthcare costs, impacting the overall economy through lost productivity and decreased workforce participation.
Vaccine Funding Levels Across US States
| State | Vaccine Funding (Estimated) | Vaccination Rate (Estimated) |
|---|---|---|
| Texas | $X million | Y% |
| California | $Z million | W% |
| New York | $A million | V% |
| … | … | … |
Note: This table is illustrative and requires actual data to be truly informative. The values (X, Y, Z, W, V, A) are placeholders and should be replaced with accurate data.
Long-Term Effects of Reduced Vaccine Funding
Reduced vaccine funding can have profound long-term effects on public health. Research suggests a correlation between decreased vaccination rates and an increase in the incidence of vaccine-preventable diseases. This, in turn, can lead to long-term health complications, disability, and even death. Furthermore, the strain on healthcare systems can create a backlog in care for other conditions, impacting the overall well-being of the population.
Reduced funding for vaccination programs can have a cascading effect, with lasting repercussions for public health and the economy. Historical data and epidemiological studies provide valuable insights into the long-term effects of reduced vaccination coverage.
Factors Contributing to the Outbreak
The recent measles outbreak in Texas, and the potential for similar outbreaks nationwide, highlights a complex interplay of factors. These factors extend beyond simple vaccine resistance and encompass a web of social, cultural, and systemic issues that contribute to preventable illnesses. Understanding these complexities is crucial for developing effective strategies to curb future outbreaks.The resurgence of measles underscores the urgent need to address the underlying causes driving vaccine hesitancy and the challenges associated with ensuring equitable access to vaccination services.
This requires a multifaceted approach, acknowledging the influence of misinformation, geographical disparities, and social norms. The Texas outbreak serves as a stark reminder that public health is not a localized concern but a collective responsibility demanding a comprehensive understanding of the contributing factors.
Misinformation and Vaccine Hesitancy
Misinformation and vaccine hesitancy are significant factors influencing vaccination rates. Dissemination of false or misleading information regarding vaccines through social media, online forums, and anti-vaccine groups has eroded public trust in the safety and efficacy of vaccines. This has led to a decline in vaccination coverage, creating vulnerable populations susceptible to preventable diseases. Studies have demonstrated a correlation between exposure to anti-vaccine narratives and lower vaccination rates.
For instance, the spread of unfounded claims about adverse reactions to vaccines can fuel anxieties and create barriers to vaccination.
Accessibility to Vaccination Services and Geographical Factors
Geographical disparities in access to vaccination services contribute significantly to outbreaks. Rural communities, low-income areas, and communities with limited healthcare infrastructure often experience difficulties in accessing vaccination clinics. Transportation challenges, lack of awareness about vaccination opportunities, and inadequate healthcare access create significant barriers. Geographic factors, such as remoteness or lack of public transportation, can limit access to vaccination services.
For example, a community without readily available vaccination clinics might have a lower vaccination rate compared to a community with easily accessible services.
Social and Cultural Factors Influencing Vaccination Decisions
Social and cultural factors play a crucial role in shaping vaccination decisions. Cultural beliefs, religious convictions, and personal experiences can influence individuals’ perceptions of vaccination. Some cultural groups may have specific concerns or beliefs about vaccines that hinder their adoption of vaccination practices. Understanding these nuances is vital for tailoring public health campaigns to effectively address concerns and build trust within diverse communities.
For example, educational campaigns should be sensitive to different cultural contexts and perspectives to enhance their effectiveness.
Role of Healthcare Providers in Promoting Vaccination
Healthcare providers play a critical role in promoting vaccination and addressing concerns. Open communication and clear explanations about the benefits and safety of vaccines can address parental and individual anxieties. Providers can educate patients about the risks of vaccine-preventable diseases and offer personalized advice tailored to individual needs and concerns. Building trust and rapport with patients is essential for fostering open dialogue and promoting vaccination.
For example, providing accurate information about the safety and efficacy of vaccines and addressing specific concerns directly can encourage vaccination.
Public Health Campaigns in Texas and Other States
Public health campaigns in Texas and other states vary in their approaches to address misinformation. Some states have focused on targeted outreach to specific communities with high levels of vaccine hesitancy, while others have employed broader campaigns aimed at educating the general public. Texas’ approach may be compared to other states’ strategies, such as those focusing on community engagement and partnerships with faith-based organizations.
Differences in strategies may reflect varying levels of vaccine hesitancy and community characteristics within each state. Comparing the success rates and community impact of these approaches could offer valuable insights for improving future campaigns.
Potential Barriers to Vaccination Access in Texas Communities
| Community Type | Potential Barriers |
|---|---|
| Rural Communities | Limited transportation options, lack of accessible clinics, lower healthcare provider density |
| Low-Income Communities | Financial constraints for transportation and clinic visits, lack of awareness about vaccination opportunities |
| Immigrant Communities | Language barriers, cultural differences in healthcare practices, mistrust of healthcare systems |
| Communities with Limited Healthcare Infrastructure | Inadequate healthcare access, insufficient resources for vaccination programs |
| Communities with High Levels of Vaccine Hesitancy | Misinformation circulating within communities, fear of adverse reactions to vaccines |
Public Health Strategies for Prevention: Measles Exploded In Texas After Stagnant Vaccine Funding New Cuts Threaten The Same Across The Us
The recent measles outbreak in Texas, tragically amplified by stagnant vaccine funding, underscores the critical need for robust public health strategies. These strategies must encompass proactive measures to prevent future outbreaks and address the underlying factors contributing to vaccine hesitancy and inadequate access. A multi-pronged approach involving community engagement, improved access, and effective communication is essential to safeguarding public health.Public health officials play a pivotal role in implementing vaccination programs.
They are responsible for overseeing the logistics of vaccine distribution, ensuring vaccine safety, and tracking the effectiveness of vaccination campaigns. This includes establishing partnerships with healthcare providers, pharmacies, and community organizations to facilitate vaccination efforts. Their expertise in epidemiology is critical for identifying and responding to outbreaks promptly. Furthermore, public health officials can educate the public about the importance of vaccination and address misinformation.
Role of Public Health Officials in Vaccination Programs
Public health officials are instrumental in coordinating and implementing vaccination programs. Their responsibilities include monitoring vaccine supply, ensuring proper storage and handling, and collaborating with healthcare providers to administer vaccinations. They also play a crucial role in surveillance and response to outbreaks, using data to identify trends and implement targeted interventions. This proactive approach is crucial for preventing widespread disease.
The measles outbreak in Texas, fueled by stagnant vaccine funding, is a serious concern, and new cuts threaten the same across the US. While local communities like Brentwood are focusing on positive developments and future plans, as highlighted by their leaders in this article brentwood leaders highlight achievements future plans for city , the lack of investment in preventative measures like vaccinations could unfortunately lead to similar outbreaks in other areas.
It’s a stark reminder that public health initiatives require sustained support to prevent serious consequences.
Importance of Community Engagement in Addressing Vaccine Hesitancy
Community engagement is paramount in addressing vaccine hesitancy. Public health officials must actively listen to community concerns and address misinformation with accurate information. This involves partnering with community leaders, faith-based organizations, and local influencers to build trust and promote vaccination. By understanding the specific concerns of different community groups, targeted interventions can be developed and implemented effectively.
For example, workshops and town halls can be organized to facilitate dialogue and answer questions.
Strategies to Improve Vaccine Access and Affordability
Improving vaccine access and affordability is essential for ensuring equitable protection against preventable diseases. This involves expanding vaccination programs to underserved communities and exploring options for reducing the financial burden of vaccinations. Public-private partnerships can play a vital role in increasing access to vaccines in areas with limited resources. Additionally, exploring subsidies or financial assistance programs can make vaccines more affordable for families.
Potential for School-Based Vaccination Programs
School-based vaccination programs can significantly enhance vaccination rates. These programs can integrate vaccination into routine health screenings and address vaccine hesitancy by offering convenient access to vaccines. They also have the potential to reach a large segment of the population at a critical time in their lives. Collaboration with school administrators and healthcare providers is crucial for successful implementation.
Effective Communication of Public Health Messages
Effective communication is crucial for disseminating accurate information about measles and vaccination. This includes tailoring messages to diverse demographics, using various communication channels, and addressing concerns in a sensitive and empathetic manner. Utilizing social media platforms, community events, and local media can reach wider audiences. For example, creating culturally sensitive materials and utilizing community language interpreters can significantly improve the effectiveness of public health messages.
Potential Partnerships between Public Health Officials and Community Organizations
| Public Health Officials | Community Organizations | Potential Partnership Activities |
|---|---|---|
| Disease surveillance and outbreak response | Community health centers | Joint outreach programs, data sharing, and resource coordination |
| Vaccine education and promotion | Faith-based organizations | Community events, faith-leader workshops, and targeted messaging |
| Logistics and distribution | Local pharmacies | Vaccine clinics in convenient locations, outreach to mobile populations |
| Data collection and analysis | Community leaders | Feedback mechanisms, community input on program design |
| Resource allocation and funding | Nonprofit organizations | Grant opportunities, fundraising initiatives, and leveraging expertise |
Potential Long-Term Effects
Measles, while often perceived as a childhood illness, can have profound and lasting consequences, particularly for vulnerable individuals. The recent surge in Texas and the potential for similar outbreaks nationwide necessitate a careful consideration of the long-term impacts on public health and healthcare systems. These effects extend far beyond the initial infection, impacting individuals, communities, and the overall healthcare infrastructure.The long-term consequences of a measles outbreak are multifaceted and far-reaching.
Beyond the immediate health concerns, the financial burden on individuals and healthcare systems is substantial, requiring careful planning and proactive measures. Understanding the potential for long-term complications, especially in vulnerable populations, is critical for developing effective prevention strategies. Drawing lessons from past outbreaks will help inform current responses and future preparedness.
Long-Term Health Impacts on Individuals
Measles, though often associated with a relatively short illness, can have lasting effects on the health of those infected. Substantial complications can arise, particularly in vulnerable populations, such as infants, the elderly, and those with compromised immune systems. These individuals are at increased risk of developing severe complications and long-term health problems. These problems can include encephalitis (inflammation of the brain), pneumonia, and even death.
In addition to the immediate health risks, the psychological impact of such an illness can be significant, affecting the patient’s quality of life and long-term well-being.
Impact on Healthcare Costs and Resources
Measles outbreaks strain healthcare resources and incur substantial costs. The need for increased hospitalizations, intensive care, and specialized treatments puts a significant financial burden on healthcare systems. The cost of treating complications and long-term sequelae, such as hearing loss or neurological damage, can extend over many years. Additionally, the need for increased staff, testing, and monitoring adds to the financial strain on already stretched resources.
This financial strain can hinder the ability of healthcare systems to address other crucial public health concerns.
Potential for Long-Term Complications, Especially in Vulnerable Populations
Vulnerable populations, including infants, pregnant women, and those with weakened immune systems, are disproportionately affected by measles. These individuals are more susceptible to severe complications and long-term health problems. Measles can lead to severe pneumonia, encephalitis, or hearing loss. The long-term implications for these populations can be devastating, impacting their ability to participate fully in daily life and affecting their overall well-being.
Examples of Past Outbreaks and Their Community Impacts
Past measles outbreaks, even in areas with robust vaccination programs, have demonstrated the devastating impact on communities. Cases of the measles in communities with low vaccination rates have led to widespread outbreaks. The 2019 measles outbreak in the United States serves as a stark reminder of the importance of maintaining high vaccination coverage. The resulting burden on healthcare resources, including hospital beds, staff, and medical supplies, highlights the critical need for proactive measures to prevent future outbreaks.
Importance of Ongoing Monitoring and Surveillance
Proactive and ongoing surveillance of vaccine-preventable diseases is essential for identifying and addressing outbreaks early. Monitoring vaccination rates, reporting cases promptly, and implementing rapid response strategies are crucial to mitigating the long-term impact of outbreaks. The collection and analysis of data on disease prevalence, vaccination coverage, and population demographics are essential for effective public health planning and resource allocation.
This data-driven approach allows for informed decision-making, targeted interventions, and ultimately, better outcomes for affected populations.
Potential Long-Term Consequences of a Prolonged Measles Outbreak in Texas
| Category | Potential Long-Term Consequences |
|---|---|
| Individual Health | Hearing loss, encephalitis, pneumonia, neurological damage, increased risk of other infections, decreased quality of life |
| Healthcare System | Increased hospitalizations, intensive care needs, specialized treatments, strain on staff and resources, long-term care requirements |
| Community Impact | Economic burden on families, disruption of educational activities, loss of productivity, decreased social participation, increased healthcare costs, psychological toll on individuals and families |
| Public Health | Decreased public trust in healthcare systems, erosion of public health infrastructure, reduced vaccination rates, potential for resurgence of other vaccine-preventable diseases |
Closure
The measles outbreak in Texas serves as a cautionary tale, highlighting the devastating consequences of underfunded public health initiatives. The interconnectedness of vaccine funding, community health, and national well-being is clear. This situation underscores the need for comprehensive strategies that address both funding gaps and misinformation, ensuring equitable access to life-saving vaccinations. Ultimately, the future of public health depends on a collective commitment to robust preventative measures.