Medical Schools Primary Care Pipeline A Deep Dive
With medical schools primary care pipeline at the forefront, this exploration delves into the crucial factors shaping the future of primary care physicians. We examine the current state of the pipeline, analyzing historical trends, regional variations, and the critical challenges facing medical schools in nurturing primary care specialists. The discussion further investigates the factors influencing the pipeline’s capacity, from financial incentives to societal perceptions, and proposes strategies to strengthen the pipeline for the future.
Successful programs and potential solutions will be presented, highlighting the importance of this vital component of the healthcare system.
This in-depth analysis will assess the current state of primary care training programs, examining enrollment trends, curriculum content, and practical training opportunities. We’ll look at successful programs and identify areas where improvements are needed. The impact of financial incentives, societal perceptions, and burnout will be explored, alongside the influence of technology and automation on the primary care physician workforce.
The discussion will also consider the future projections of primary care needs and the potential role of emerging technologies and interprofessional collaboration.
Current State of Primary Care Pipeline
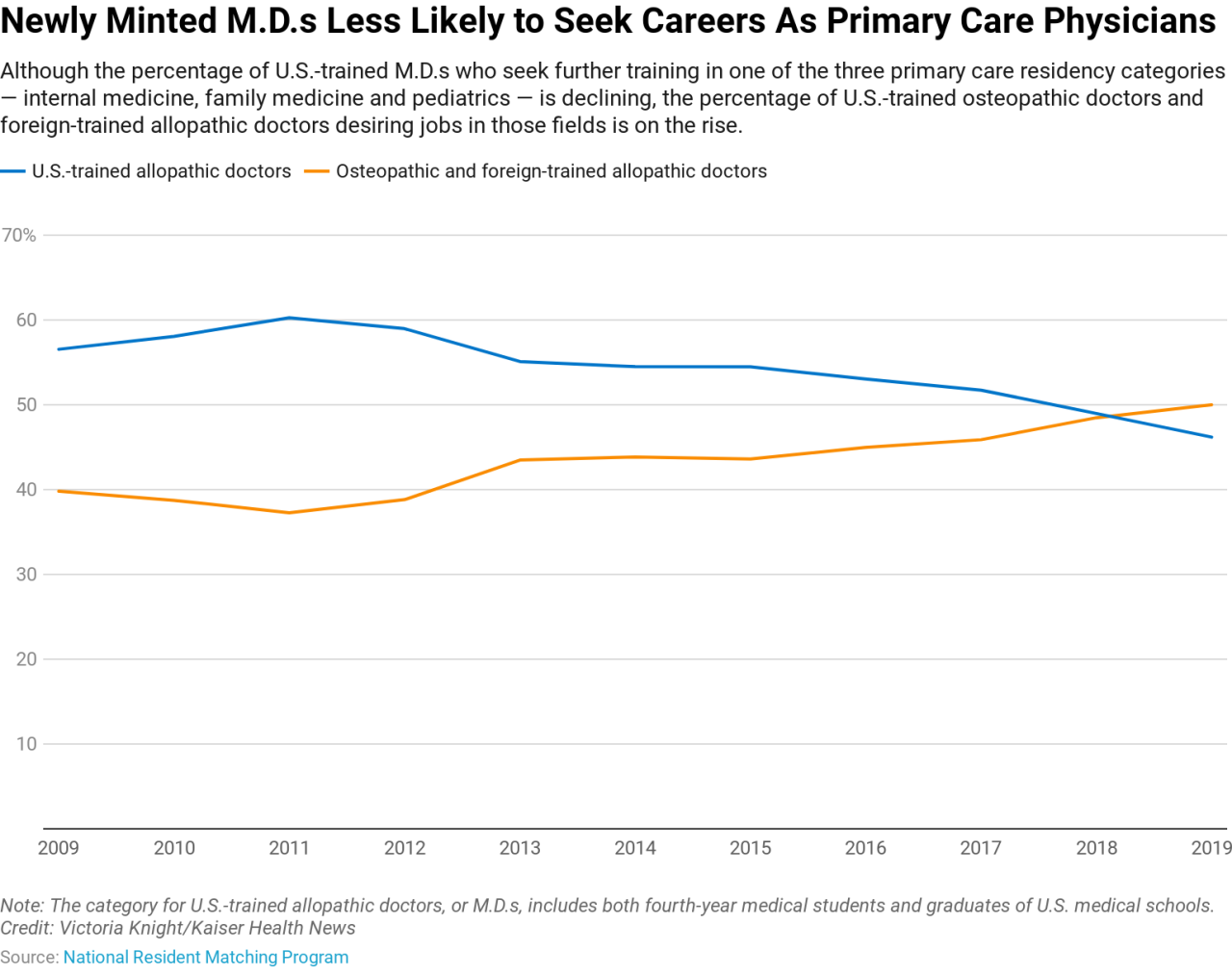
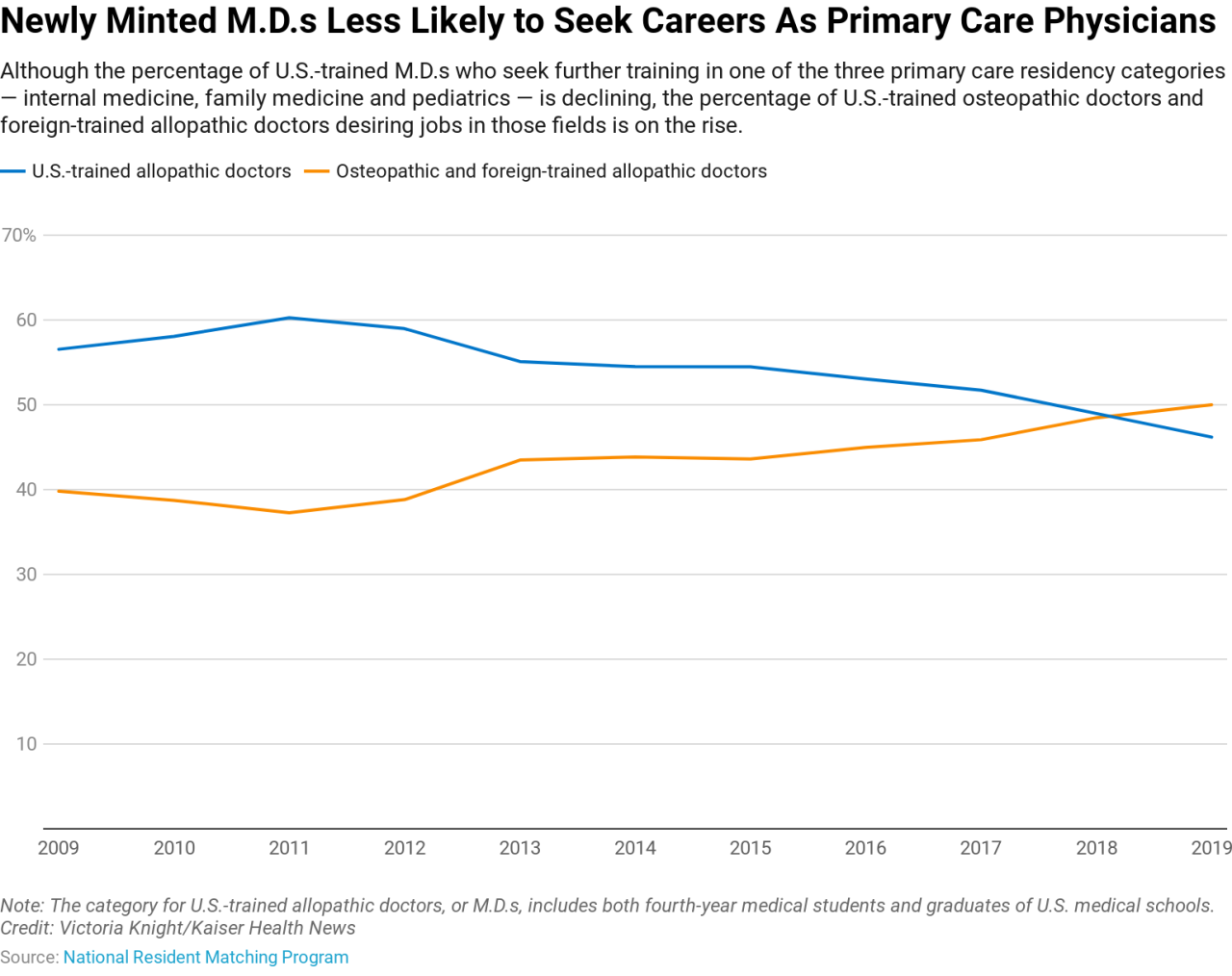
The primary care physician pipeline, crucial for providing accessible and affordable healthcare, faces significant challenges. Historically, primary care has often been perceived as less prestigious than other specialties, leading to a decline in medical students choosing this path. This, coupled with financial and societal factors, has contributed to a strained primary care workforce, particularly in underserved areas. Understanding the current state, including historical trends and regional variations, is essential for implementing effective solutions.
Historical Overview of the Primary Care Physician Pipeline
Historically, primary care has experienced fluctuations in enrollment and graduation rates. In some eras, primary care was a more common choice for medical students, reflecting societal needs and values. However, as specialization became more prominent and lucrative, the number of students opting for primary care decreased. Data from various medical schools reveals a downward trend in the number of students pursuing primary care training.
Graduation rates, while varying, often correlate with the number of students entering the specialty, mirroring the historical shifts in medical school curriculum and societal perceptions.
Current Challenges and Limitations
Several factors contribute to the current limitations of the primary care pipeline. Financial incentives for specialization often outweigh those for primary care. This disparity, coupled with the perceived prestige associated with certain specialties, dissuades many students from choosing primary care. Moreover, the rising cost of medical education and the increasing burden of student loan debt further influence students’ choices.
This results in a disproportionate shortage of primary care physicians, particularly in rural and underserved areas.
Regional Variations in the Primary Care Pipeline
The primary care pipeline differs significantly across various regions and countries. Access to quality primary care varies greatly depending on the availability of physicians and resources. Training models differ, with some countries emphasizing community-based learning and others prioritizing hospital-based experiences. Incentive programs for primary care physicians also vary considerably. In some regions, robust financial incentives and subsidies encourage medical students to pursue primary care, while other regions lack such support.
Key Factors Contributing to the Current State
Several key factors influence the current state of the primary care pipeline. The financial incentives for specialization often outweigh those for primary care, which contributes to the perception of primary care as a less lucrative career path. The perceived prestige associated with certain specialties also plays a significant role. Societal influences, such as the media’s portrayal of certain medical professions, can also shape student choices.
Addressing these factors requires a multifaceted approach, including financial incentives, educational reforms, and broader societal shifts in perceptions of primary care.
Successful Primary Care Training Programs and Initiatives
Several successful primary care training programs and initiatives have been implemented to address the challenges in the primary care pipeline. These initiatives often involve a combination of financial incentives, enhanced training models, and community-based learning experiences. For instance, some medical schools have implemented dedicated primary care tracks within their curriculum, providing focused training in this area. Examples of successful programs include those emphasizing early exposure to primary care through clerkships and rotations in community settings.
Comparison of Primary Care Training Curricula
| Medical School | Primary Care Focus Hours | Rotation Details |
|---|---|---|
| Example School A | 1000 hours | Detailed description of rotations, including a dedicated primary care track with exposure to diverse patient populations, and a strong emphasis on preventative care and chronic disease management. |
| Example School B | 800 hours | Rotations are structured to include a focus on primary care, but with less emphasis on a dedicated track, with a mix of hospital and community-based experiences. |
Note: This table provides a simplified comparison and does not include all medical schools. Data for specific schools may vary, and the content within “Rotation Details” columns should be further expanded to include detailed information about the rotations. A comprehensive analysis would require access to detailed curricula from numerous institutions.
Factors Affecting Pipeline Capacity
The primary care physician pipeline, crucial for maintaining accessible and quality healthcare, faces numerous challenges. Understanding these factors is essential to developing effective strategies for recruitment and retention. The current landscape presents both opportunities and obstacles, demanding a multifaceted approach to bolstering the primary care workforce.
The primary care pipeline in medical schools is crucial for future healthcare access, but the current political climate presents some serious roadblocks. For example, the recent wave of deportations and the broader issue of immigration policy, like the ones discussed in abcarian trumps deportations threaten california economy built on hypocrisy , threaten the economic well-being of California, a state heavily reliant on immigrant labor.
This, in turn, could impact the overall availability of resources needed to support the medical schools primary care pipeline. It’s a complex issue, but one we need to address.
Financial Incentives and Reimbursement Models
Financial incentives play a significant role in medical students’ career choices. Attractive reimbursement models for primary care services can motivate future physicians to pursue these specializations. Conversely, if reimbursement structures do not adequately compensate for the time and effort required, primary care may become less appealing. For example, if a particular model of care is less profitable, it may lead to a decrease in the number of physicians in that area of medicine.
This could have a domino effect on the patient experience. The complex interplay between financial incentives and career choices warrants careful consideration to ensure that primary care remains a viable and rewarding option.
Societal Perceptions and Career Prestige
Societal perceptions of primary care significantly influence medical students’ career paths. If primary care is viewed as less prestigious or less lucrative than other specialties, fewer students may opt for it. This is not simply about the image of the profession but also the social standing associated with the job and how people perceive it. These perceptions can be influenced by various factors, such as media portrayals and cultural norms.
To address this, a concerted effort to highlight the vital role of primary care physicians in preventative care and community health is crucial.
Physician Burnout and Stress
Physician burnout and stress are significant factors affecting the primary care pipeline. The demanding nature of primary care, including long hours, administrative burdens, and patient expectations, can lead to burnout and decreased job satisfaction. This can ultimately lead to doctors leaving the field and affecting the pipeline. Strategies to mitigate burnout, such as improved work-life balance policies, adequate staffing levels, and support systems, are essential to ensure the long-term sustainability of the primary care workforce.
Technology and Automation
Technological advancements and automation are impacting the primary care physician workforce in several ways. While technology can streamline certain tasks and improve efficiency, concerns exist regarding the potential for deskilling or the displacement of human interaction. Furthermore, there are concerns about the equitable access to and utilization of technology in different primary care settings. A nuanced understanding of how technology can be integrated to enhance, not replace, the role of the physician is critical.
This includes training physicians on new technologies and ensuring equitable access to necessary resources.
Accessibility of Primary Care Training and Education
The accessibility of primary care training and education is a key component in the pipeline’s capacity. Unequal distribution of residency programs, disparities in funding for training, and limited opportunities in underserved areas can significantly impact the availability of primary care physicians in these regions. Analyzing the distribution of training programs across different geographic areas, along with an assessment of the availability of funding and resources, can identify and address these inequities.
It is important to examine the geographic distribution of training programs and assess the resources available in different regions to determine how to address these inequalities.
Physician Compensation Models
| Model | Salary Structure | Benefits |
|---|---|---|
| Model A (Salaried Position) | Fixed annual salary, potentially with performance-based bonuses. | Comprehensive benefits package including health insurance, retirement plans, paid time off, and professional development opportunities. |
| Model B (Fee-for-Service) | Payment based on the services rendered to patients. Potential for higher earnings with high patient volume. | Benefits package often varies, but can include health insurance and retirement plans, though these may be less comprehensive than salaried models. |
| Model C (Hybrid Model) | A combination of salary and fee-for-service components. | Benefits packages can be tailored based on the specific structure of the model. |
Different compensation models influence the attractiveness of primary care. Understanding the pros and cons of each model, including factors like potential earnings, stability, and associated benefits, is vital for creating a supportive and competitive environment. For instance, a salaried model can offer greater stability, while a fee-for-service model may allow for higher earning potential.
Strategies to Enhance the Pipeline
Attracting and retaining primary care physicians is crucial for a robust and accessible healthcare system. A strong primary care pipeline ensures that communities have access to essential medical services, fostering preventative care and improving overall health outcomes. This section explores strategies to enhance the medical student pipeline, improve compensation, and foster a supportive learning environment.Addressing the current challenges requires a multi-faceted approach that targets students, educators, and policymakers.
This includes strategies to make primary care more attractive, to alleviate financial pressures, and to enhance the educational experience to ensure future physicians are well-equipped to meet the needs of patients and communities.
Improving the medical schools primary care pipeline is crucial, and one aspect of this involves streamlining administrative tasks. Think about how much time and effort could be saved if crucial services automatically launched when the system boots, like a properly configured Linux system. For example, using a method like those described in this helpful guide on how to auto start services on boot in linux , we could free up valuable resources for doctors and staff to focus on patient care.
This would significantly strengthen the overall effectiveness of the medical schools primary care pipeline.
Attracting Medical Students to Primary Care
Enhancing the appeal of primary care necessitates a shift in perception, showcasing its multifaceted nature and rewards. Highlighting the significant impact primary care physicians have on patient lives can motivate students. Experiential learning opportunities, such as shadowing or volunteering with primary care practitioners, can provide valuable insights into the daily realities and the intrinsic satisfaction of this field.
Emphasis on the long-term professional fulfillment and the opportunity for significant community impact should also be emphasized. Interactive simulations and role-playing exercises, which replicate real-world scenarios, can increase student engagement and demonstrate the complexity and variety of primary care practice.
Addressing Financial Disincentives and Improving Compensation, Medical schools primary care pipeline
Financial incentives and compensation structures play a pivotal role in attracting and retaining primary care physicians. Current models often undervalue the critical role primary care physicians play in healthcare, leading to a shortage of providers. Financial incentives for primary care physicians could include loan repayment programs, scholarships, and competitive salaries, particularly in underserved areas. These financial incentives can be tailored to specific needs and situations, such as residency training programs and loan forgiveness programs.
In addition, bundled payment models and value-based care approaches that reward high-quality primary care can improve compensation and encourage the practice of preventative care. Exploring alternative payment models and incentives is essential.
The Role of Mentorship and Leadership
Mentorship and leadership play a crucial role in shaping career choices and influencing professional development. Pairing medical students with experienced primary care physicians, who can serve as role models and provide guidance, is essential. Mentors can offer insights into the practical aspects of primary care, addressing any potential concerns and dispelling myths about the profession. Leadership opportunities, such as student-led primary care clinics or research projects, can foster leadership skills and provide invaluable experience.
Creating opportunities for students to engage with primary care leaders and learn about their career journeys can be highly effective.
Improving Primary Care Training Curriculum in Medical Schools
Medical school curricula must be redesigned to incorporate a robust primary care focus. The current curriculum should be supplemented with more extensive training in primary care skills and competencies, from basic clinical procedures to chronic disease management. Experiential learning, including community health projects and exposure to diverse patient populations, should be prioritized. This will enhance students’ understanding of primary care’s importance in the broader healthcare context and the diverse range of patients.
Integrating interprofessional education, where students learn from other healthcare professionals, can broaden perspectives and strengthen collaborative practice.
Fostering a Supportive and Engaging Learning Environment
Creating a supportive and engaging learning environment is critical for students’ interest in primary care. Creating opportunities for students to interact with primary care physicians and explore the realities of primary care practice is crucial. Positive feedback and constructive criticism are essential elements in creating a supportive environment. A focus on well-being and stress management can improve the student experience, especially in demanding fields like medicine.
Creating a culture of mutual respect and collaboration can also increase engagement.
Potential Funding Models for Primary Care Education and Training Programs
| Funding Model | Description | Target Audience |
|---|---|---|
| Model A: Public-Private Partnerships | Collaboration between government agencies and private foundations to provide grants and scholarships for primary care training programs. These grants may be awarded to medical schools or community health centers. | Medical schools, community health centers |
| Model B: Value-Based Reimbursement | Primary care physicians receive a portion of the savings generated from improved health outcomes and reduced hospitalizations, motivating them to focus on preventive care and holistic patient management. | Primary care physicians |
| Model C: Targeted Grant Programs | Grants specifically designed to support underserved areas or communities with limited access to primary care, fostering infrastructure and training for primary care physicians. | Medical schools, community health centers, underserved communities |
Future Directions and Projections
The future of primary care is poised for significant transformation, driven by evolving demographics, technological advancements, and a growing recognition of the importance of interprofessional collaboration. Understanding these forces is crucial to ensuring a robust and responsive primary care system that meets the needs of a changing population. This section will explore the future landscape, anticipating needs, and considering how to best prepare for it.Predicting the precise future of primary care is challenging, but based on current trends and projections, we can anticipate significant changes in the coming years.
These changes will be driven by shifts in population demographics, the increasing prevalence of chronic conditions, and the ever-evolving role of technology.
Projecting Future Needs for Primary Care Physicians
Primary care physicians will be increasingly needed to address the health needs of an aging population, the rise of chronic diseases, and the growing demand for preventative care. Demographic shifts, such as a growing elderly population and increasing diversity, will necessitate a workforce capable of addressing the specific health needs of these diverse groups. For instance, the growing Hispanic population in the US will require primary care physicians fluent in Spanish to meet the healthcare needs of this community effectively.
The medical schools’ primary care pipeline is a crucial area of focus, especially given the ongoing need for doctors in underserved communities. Tragically, recent events like the tornadoes touching down around Houston, killing 1 ( tornadoes touch down around houston killing 1 ), highlight the importance of a strong and resilient healthcare system. Ultimately, bolstering the primary care pipeline is vital to ensuring adequate medical care for all, regardless of circumstance.
Potential Impact of New Technologies and Advancements
Technological advancements, such as telehealth, artificial intelligence (AI), and wearable technology, are poised to revolutionize primary care. Telehealth is already proving invaluable in expanding access to care, particularly in rural and underserved areas. AI can assist with diagnostics, personalized treatment plans, and administrative tasks, potentially freeing up physicians’ time for patient interaction. Wearable technology can help patients monitor their health, enabling proactive interventions and better self-management of chronic conditions.
Importance of Interprofessional Collaboration in Primary Care
Effective primary care increasingly relies on interprofessional collaboration. Teams involving physicians, nurses, social workers, pharmacists, and other healthcare professionals can offer a more comprehensive and holistic approach to patient care, addressing social determinants of health and fostering better patient outcomes. The integration of these diverse perspectives allows for a deeper understanding of the patient’s complete needs, moving beyond a purely biomedical focus.
Emerging Roles and Responsibilities for Primary Care Physicians
Primary care physicians will be expected to adapt to new roles and responsibilities, encompassing a broader range of skills and responsibilities. These include:
- Acting as patient navigators, guiding patients through complex healthcare systems.
- Providing care coordination, managing multiple health conditions for complex patients.
- Integrating technology into practice, utilizing telehealth and AI tools effectively.
- Emphasizing preventative care, focusing on health promotion and disease prevention.
- Addressing social determinants of health, such as housing, food security, and transportation.
Potential Policy Changes to Support the Primary Care Pipeline
Policy changes are necessary to support the primary care pipeline and ensure a sufficient number of qualified physicians to meet future needs. These include:
- Increasing funding for primary care training programs.
- Providing loan repayment programs to attract and retain primary care physicians in underserved areas.
- Expanding recruitment efforts to increase diversity in the primary care workforce.
- Streamlining the licensing and credentialing process for physicians.
How Community Health Centers Can Support the Primary Care Pipeline
Community health centers (CHCs) play a vital role in supporting the primary care pipeline. They provide training opportunities for medical students and residents, offering hands-on experience in diverse patient populations and practice settings. They can also offer scholarships and financial support to aspiring primary care physicians. Furthermore, CHCs often serve as a bridge between the academic and community settings, helping to ensure a workforce equipped to address the specific needs of underserved communities.
Telehealth in Primary Care Education and Training
Telehealth offers unique opportunities for primary care education and training. It allows students and residents to gain experience with diverse patient populations and practice settings, particularly in rural and underserved areas. Simulations and virtual patient encounters can enhance learning and provide opportunities for feedback and practice.
Table of Technologies in Primary Care
| Technology | Description | Impact on Primary Care |
|---|---|---|
| Telehealth | Remote delivery of healthcare services using technology, including video conferencing, messaging, and remote monitoring. | Increased access to care, particularly for patients in rural areas or with mobility limitations; allows for more efficient scheduling and reduced travel time for patients. |
Illustrative Examples of Primary Care Success
The primary care physician pipeline faces persistent challenges, but successful programs demonstrate effective strategies for nurturing future providers. Examining these programs offers valuable insights into building robust and resilient primary care systems. These models can inspire other institutions and communities to create similar structures.Successful primary care programs aren’t one-size-fits-all; they are tailored to specific needs and contexts. However, key elements often recur, including innovative curriculum designs, strong mentorship programs, and supportive community partnerships.
The programs detailed below illustrate how these elements can yield positive results for both patients and providers.
The “Rural Access Initiative” Program
This program focuses on addressing the critical shortage of primary care physicians in rural communities. Recognizing that rural areas often lack access to specialized care, the program aims to cultivate a pipeline of physicians committed to serving these underserved populations.
- Curriculum Emphasis: The curriculum incorporates dedicated modules on rural health, cultural competency, and community engagement. Students are exposed to the unique challenges and rewards of rural practice through simulation exercises, community visits, and shadowing experiences in rural clinics. Students also participate in workshops on financial planning for rural practice.
- Mentorship and Support: The program features a robust mentorship program, connecting students with experienced rural primary care physicians. Mentors provide guidance on navigating rural practice, offer insights into community resources, and support professional development.
- Community Partnerships: The program actively collaborates with rural healthcare organizations and community leaders. This collaborative approach fosters a sense of belonging and promotes long-term physician retention in the area.
- Financial Incentives: The program provides financial incentives to students committed to practicing in rural areas after graduation. This includes loan repayment assistance and scholarship opportunities.
Positive Outcomes
The Rural Access Initiative has demonstrated significant positive outcomes. Patient satisfaction scores have improved markedly, as evidenced by surveys and feedback forms. Physician satisfaction rates are also high, with a significant percentage of graduates reporting a strong sense of fulfillment in their chosen field.
Program Structure
The program’s structure is visualized below.
| Component | Description |
|---|---|
| Curriculum | Focused on rural health, cultural competency, and community engagement. |
| Mentorship | Robust program linking students with experienced rural physicians. |
| Community Partnerships | Collaboration with rural healthcare organizations and community leaders. |
| Financial Incentives | Loan repayment assistance and scholarship opportunities. |
The program’s success highlights the importance of addressing the needs of rural communities and fostering a culture of support and mentorship.
Final Summary: Medical Schools Primary Care Pipeline
In conclusion, the medical schools primary care pipeline faces complex challenges, requiring multifaceted solutions. Strengthening the pipeline necessitates addressing financial disincentives, fostering a supportive learning environment, and enhancing the curriculum to attract and retain talented individuals in primary care. Ultimately, a robust primary care pipeline is crucial for ensuring accessible, high-quality healthcare for all. The future of primary care hinges on these proactive measures, fostering a sustainable and thriving system of primary care physicians for the benefit of patients and the healthcare community.